skills for carers
This section covers:
- Why is Change so Difficult? - Introducing the Circle of Change
- Motivational Interviewing and Reflective Listening
WHY IS CHANGE SO DIFFICULT?
"Consider how hard it is to change yourself and you'll understand what little chance you have in trying to change others ”
― Jacob M. Braude
"People underestimate their capacity for change,
"There is never a right time to do a difficult thing"
― John Porter
"The secret of change is to focus all of your energy, not on fighting the old, but on building the new."
― Socrates
"When one door closes, another opens; but we often look so long and so regretfully upon the closed door that we do not see the one that has opened for us."
― Alexander Graham Bell
The internet is littered with quotes about change and why change is needed, everything from productivity at work to personal development and changing patterns of behaviour to 'improve' our lives. This just illustrates that 'change' in any context is not easy.
CHANGE AND EATING DISORDERS
With an eating disorder the patient becomes trapped within behaviours that fuel the eating disorder. What starts as a coping strategy eventually causes more problems than it solves. The patient stubbornly resists any idea about change, they see no need for change. The low weight of an anorexia sufferer itself leads to changes in thinking and behaviour which perpetuate the illness.
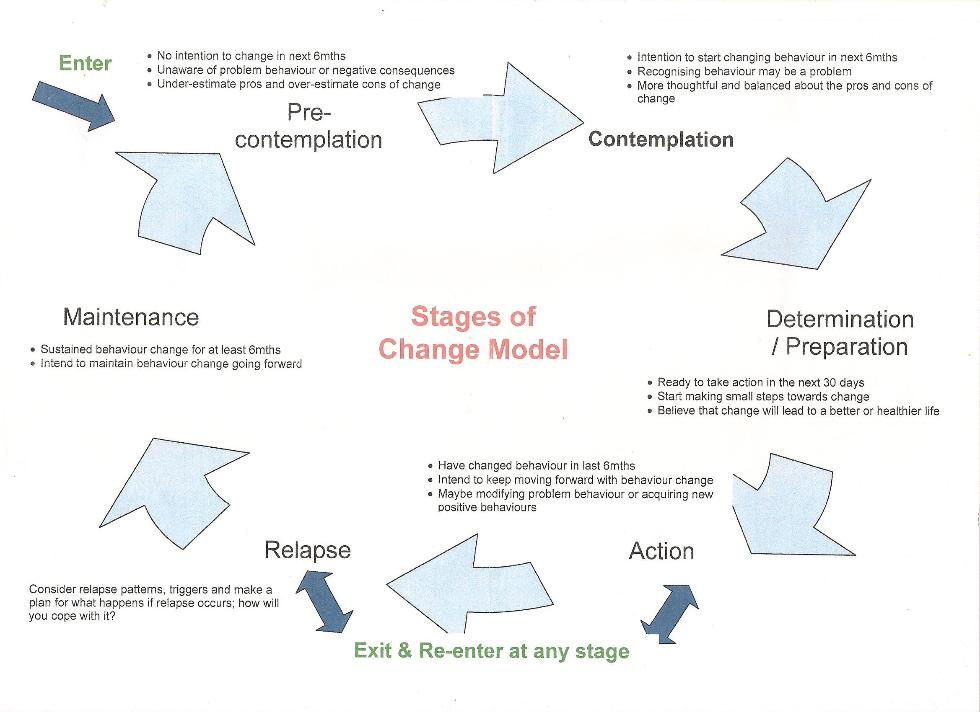
Changing eating disorder behaviours is therefore a complex process and consists of several stages that the patient goes through. It can be helpful to think of these stages in a circle, in which it is possible to move both forwards and backwards. See diagram.
STAGES OF CHANGE
Pre-contemplation
The patient does not acknowledge there is any need to change behaviour despite concern expressed by family and friends. There may be an under-estimating of pros and over-estimating of cons of change. There is no intention to change.
Contemplation
This next stage involves recognising that behaviour may be a problem but the patient may be 'in two minds' about the need to change. There is a more thoughtful and balanced view about the pros and cons of change.
Determination / Preparation
The patient is now ready to take action and believes that change will lead to a better or healthier life, ready to start making small steps towards change.
Action
The beginning of real change. Behaviours have changed in the last six months and the intention is to keep moving forward.
Relapse
Developing new connections with the world without the eating disorder takes time and effort and there may be setbacks. Relapse patterns and triggers should be considered.
Maintenance
Sustained behaviour change for at least six months.
The patient may go through each stage several times before lasting progress is maintained. When setbacks occur try not to be too discouraged, this is part of the illness pattern. New things are learnt with each setback and restart.
There is no set timescale, each person is an individual and will have to work through their illness at their own pace. It can be difficult to stay positive and supportive when your child or loved one seems to be stuck in the pre-contemplation stage.
There is psychological research evidence on the mechanisms of change which shows that people become more ready to change if:
1. It becomes important to them, i.e. the positive benefits of change outweigh the negative aspects.
2. They are confident that they can change.
As carers, if we understand about the change mechanism we can help to move our loved ones towards change, rather than reinforcing the eating disorder behaviours. Ask the health professionals treating your loved one for guidance or training. We have reviewed on this site the CAMHS's Skills Based Group Programme for Parents which includes this.
One of the techniques which can be helpful in exploring readiness to change is a style of communication called ‘motivational interviewing’ which includes 'reflective listening'. See ‘Sources’ below for more information.
SUMMARY
Unlike most people who are ill, an eating disorder patient often will not recognise that they have a problem and will not want to change.
Expectations need to be paced with the readiness to change, carers need to remain optimistic but not too pushy.
If you feel that your loved one has become stuck speak to the health professionals treating them. A review of their treatment plan may be helpful.
Training for parents and carers can help speed up the process. What we do and say can help to move our loved ones towards change, rather than reinforcing the eating disorder behaviours. The information below on motivational interviewing and reflective listening is recommended.
This can at times be a very frustrating and tiring process for carers. Some people find it helpful to meet up with other carers in the same situation. The contact us page will have details of the next EAS-ED Support Group meeting, or find out what is available in your area.
Try and stay positive - when ready to change people do recover from eating disorders.
SOURCES:
Skillls Based Group Programme for Parents, CAMHS Eating Disorders Team, North Essex PFT.
Skills Based Learning for Caring for a Loved One with an Eating Disorder – The New Maudsley Method (Janet Treasure, Grainne Smith & Anna Crane ISBN 978-0-415-43158-3)
Motivational Interviewing & Reflective Listening
These techniques are explained with some of the other methods used at The Maudsley: http://thenewmaudsleyapproach.co.uk/index.php/test-page-1/test-sub-page/
Another very helpful site on all aspects of supporting a friend with an eating disorder, is the 'Student Minds' website. https://www.studentminds.org.uk/findsupport.html
The information on this site is not a substitute for professional advice